Favourable Conditions for Microbial Growth in Cleanroom Area
Microbial growth and contamination in sterile manufacturing area is a big issue. Microbial growth increases in sterile area due to the change in the environmental conditions.
In the pharmaceutical industry, the end is to produce a drug that will help humanity in either promotion of health status, amelioration of the disease condition or palliating a chronic illness. For this cause, the pharmaceutical companies provide for themselves a conducive place to make drugs. These special places have something in common; cleanliness and therefore called cleanroom area.
Cleanrooms are the most sterile places in drug production industry. Its function in keeping drugs as good as they should be is not to be overemphasized. But what happens if the so-called cleanroom is not sterile. What if they are contaminated by microbes? But then, what could even make microbes grow in such a sterile place. A lot of factors! You know that microbes are ubiquitous and therefore can survive in very stringent conditions. Let's examine them in very simple terms.
Relative humidity: This is the ratio of water content in an environment (humidity of a place) to that of atmospheric humidity. If the relative humidity of cleanroom at left to be high, then it will help the microbes to thrive very well. You may ask how water content affect the growth of microbes. It is due to the importance of the oxidation-reduction process. You know that in the microbial physiological process, there must be an exchange of electron transfer. So you see, how important it is.
Temperature: As a scientist, you know that sunlight is the prime of all lives but then the temperature is the perimeter of sunlight. The temperature of the environment affect the enzymatic reactions of every living organism, therefore, regulates the metabolism of microbes. All temperature range is suitable for different groups of microbes. But cleanroom should set its temperature range at extreme temperatures because there are few microbes that could thrive there.
Nutrient: All
that most microbes need is a carbon source and a small amount of nitrogen cum
other trace elements. Most pharmaceutical materials are composed of primarily
carbon element. Where the cleanroom is not clean enough or maybe containing
some debris of formulated drugs, a microbe can grow on it and multiply rapidly
to contaminant other places in the cleanroom. Another terrific thing about
microbes is that they have the ability to change five carbon compound to six
carbon compound and vice versa. Some microbes can also tolerate ethanol. Some
microbes, because they can degrade some pharmaceutical products can be found in
the cleanroom.
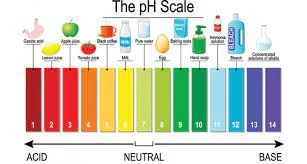
pH: This is the degree of acidity or alkalinity of a place, substance or living thing. Ideally, microbes can be divided into acid-loving, acid tolerant, basic tolerant and basic loving. The ability of a microbe to survive is dependent on the pH. If a cleanroom which supposed to be acid is eventually alkaline, it will encourage the growth of microorganisms
Oxygen: Microbes use many in the metabolism of the nutrient for the generation of energy. Aerobic microbes which are commonest in nature around human habitations need oxygen. When oxygen is sufficient in cleanroom which already had microbes, the microbes will be favored and therefore will be much contamination. Oxygen is essential because it helps microbes in the oxidation-reduction reactions.
Pressure: The pressure of a place affects the health and growth of microbes. A pressure that is very high does not encourage growth. Most times, it is recommended that cleanroom is kept under high pressure when not in use. This is to discourage the growth of microbes introduced there by workers.
In as much as we know that these factors affect the microobial contamination it is multiple hurdles in the sense that the presence of one positive factor does not guarantee the thriving of microbes if the others factors are not present or positive.





Comments
Post a Comment
If you have any doubts, please let me know